Glaucoma and intraocular pressure
- Emiliano Terán
- Mar 13, 2023
- 3 min read
Updated: Mar 14, 2023

Glaucoma is a visual disease characterized by the failure of retinal cells to transmit visual data from the eye to the brain. Glaucoma can cause irreversible vision loss if not treated on time. In this article, we will talk about the negative impact of increased intraocular pressure on ocular structures and visual function.
Glaucoma is one of the leading causes of irreversible vision loss in the US and around the world. Millions of Americans are estimated to be living with glaucoma, 2.7 million of whom are affected by its most common form, open-angle glaucoma, affecting 3.3 million Americans age 40 and older. Based on prevalence studies, 79.6 million people were expected to have glaucoma in 2020, a number likely to increase to 111.8 million people by 2040. The global prevalence of glaucoma was 3.54% (95% confidence interval: 2.09 - 5.82). The prevalence of primary open-angle glaucoma was 3.05% (95% confidence interval: 1.69 - 5.27), and the prevalence of primary spot-closure glaucoma was 0.50% (95% confidence interval: 0.11 - 1.36). .
One of the main triggers of glaucoma is the increase in intraocular pressure (IOP). The IOP is the force with which the fluid that fills the inside of the eye (vitreous humor) presses on the walls of the eye. Typical IOP values are in the range of 10 to 21 mmHg (millimeters of mercury), but can be increased by other factors, such as age, hereditary variables, use of specific medications, or serious illness.
Elevated IOP can cause mechanical pressure and torsion of the posterior structures of the eye. Particularly, of the layers of the retina that depend on blood vessels for their nutrition and oxygenation, such as the inner nuclear layer, the inner plexiform layer and the layer of nerve fibers through which the nerve threads exit (ganglion cell axons). Elevated IOP can compress these nerve fibers and weaken their capacity, resulting in visual field loss. In addition, elevated IOP can affect visual blood flow and decrease the supply of oxygen and nutrients to ganglion cells, leading to cell death from ischemia.
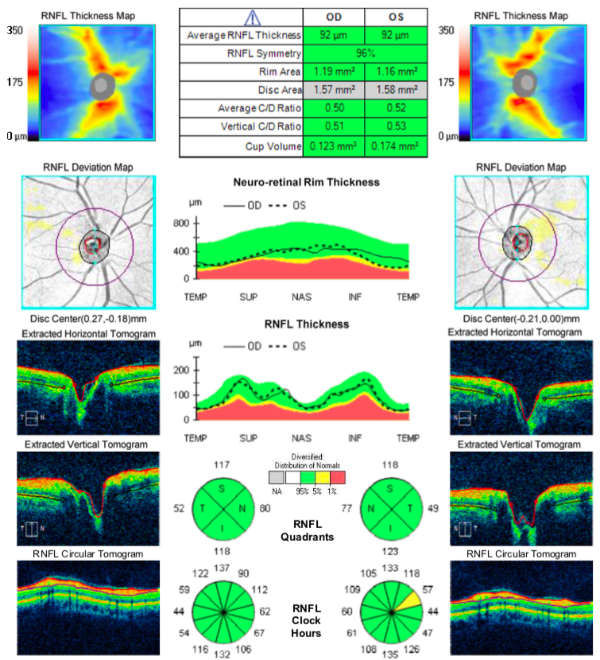
The effect of pressing on the layers of the retina can be routinely measured using an optical coherence tomograph (OCT). This device can determine the thickness of the different layers of the retina, as well as its variation along and across the fundus. An example of this evaluation can be seen in Figure 1.
The negative impact of IOP on glaucoma and visual function is neither direct nor constant. Certain individuals can develop glaucoma with normal or low IOP levels (hypotensive glaucoma), while others can withstand high levels without harm (visual hypertensives). In addition, individual factors can modify the negative effect of IOP, such as the thickness of the cornea, the size of the optic disc, or the type of nerve fibers affected.
The negative effect on visual function due to increased intraocular pressure can be estimated using a Humphrey Field test (HFT). A HFT is an instrument that is used to measure a person's visual field, that is, the area that they can see with each eye without moving their head. In Figure 2, you can see an example of his estimation. You can learn more about this instrument in one of our previous articles.

In our research team, we are conducting studies to identify this serious visual disease. We have a multidisciplinary team that is developing screening methods and computational algorithms to detect this condition. We will delve into these topics in more detail in the future.
Final comments
It is essential to undergo regular ophthalmological examinations to measure IOP and monitor the condition of the optic nerve and visual field. These important visual evaluations should be performed by trained personnel at an ophthalmological clinic. The treatment for glaucoma involves reducing IOP using ophthalmic medications, laser procedures, or obstructive inserts. To identify or manage this delicate visual disease, it's important to see a specialist.
To know more:
1. Ahmed OM, Waisbourd M, Spaeth GL, Katz LJ. Improvement in structure and visual function in patients with glaucoma: the possible key to better treatment? Surv Ophthalmol. 2021 Jul-Aug;66(4):644-652.
https://pubmed.ncbi.nlm.nih.gov/33316283/
2. Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014 May 14;311(18):1901-11.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4523637/
3. Twa, Michael D. Intraocular Pressure and Glaucoma. Optometry and Vision Science 95(2):p 83-85.
https://journals.lww.com/optvissci/Fulltext/2018/02000/Intraocular_Pressure_and_Glaucoma.1.aspx



Komentáře